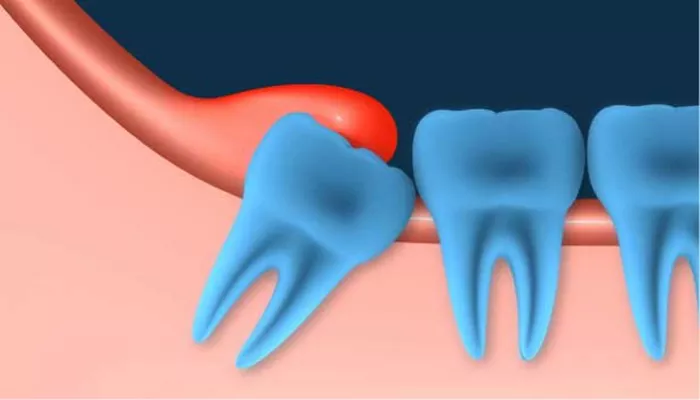
Pericoronitis Symptoms
Recognizing the symptoms of pericoronitis is essential for prompt diagnosis and treatment. Symptoms can range from mild discomfort to severe pain, depending on the severity of the condition.
1. Pain and Swelling
One of the earliest and most common symptoms is pain and swelling around the partially erupted tooth. The gums may appear red and inflamed.
2. Difficulty in Chewing
Due to tenderness and inflammation, chewing food can become uncomfortable. In severe cases, opening the mouth fully may also be difficult.
3. Bad Breath (Halitosis)
The accumulation of food particles and bacteria around the affected tooth can cause an unpleasant odor or bad taste in the mouth.
4. Gum Infection
Pericoronitis may lead to localized gum infection, with pus formation in advanced cases. This can result in a painful abscess.
5. Fever and Swollen Lymph Nodes
Severe cases of pericoronitis may cause systemic symptoms such as fever and swollen lymph nodes in the neck or jaw.
6. General Discomfort
Individuals with pericoronitis often report general discomfort, including headaches, earaches, or pain radiating to other areas of the mouth.
Pericoronitis Treatment
The treatment of pericoronitis depends on the severity of the condition. A dentist’s evaluation is critical to determine the best approach.
1. Professional Cleaning
For mild cases, a dentist may clean the area around the affected tooth. This involves removing trapped food particles and bacteria from beneath the gum flap.
2. Antibiotics
If the infection has spread or is accompanied by systemic symptoms such as fever, antibiotics may be prescribed to control the bacterial infection.
3. Pain Management
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, are often recommended to alleviate discomfort and reduce inflammation.
4. Incision and Drainage
For severe cases with pus formation, the dentist may perform an incision to drain the abscess, relieving pressure and promoting healing.
5. Gum Flap Removal
In some cases, the dentist may remove the gum flap (operculectomy) that partially covers the tooth, preventing food and bacteria from accumulating in the future.
6. Referral to a Specialist
For complicated cases, such as those involving impacted wisdom teeth, a referral to an oral surgeon for surgical intervention may be necessary.
Pericoronitis Home Remedies
While professional dental care is crucial, certain home remedies can help manage symptoms and prevent the condition from worsening until you see a dentist.
1. Warm Saltwater Rinse
Rinsing your mouth with warm salt water (1 teaspoon of salt in a glass of warm water) can reduce bacteria, soothe inflammation, and promote healing.
2. Good Oral Hygiene
Brushing and flossing gently around the affected area helps remove food particles and bacteria. Use a soft-bristled toothbrush to avoid irritating the gums further.
3. Cold Compress
Applying a cold compress to the outside of your jaw can reduce swelling and numb the area, providing temporary pain relief.
4. Over-the-Counter Medications
Non-prescription pain relievers such as ibuprofen or acetaminophen can help control pain and inflammation.
5. Avoid Irritants
Avoid consuming hard, crunchy, or spicy foods that may aggravate the sensitive gums around the affected tooth.
6. Antibacterial Mouthwash
Using an antibacterial mouthwash containing chlorhexidine can help reduce bacterial growth and minimize infection risk.
Pericoronitis Removal
When recurring pericoronitis becomes a persistent problem, removal of the affected tooth may be the most effective solution. This step is often necessary for impacted or partially erupted wisdom teeth.
1. Evaluation by a Dentist or Oral Surgeon
The dentist or oral surgeon will assess the position and condition of the tooth through clinical examination and imaging, such as X-rays.
2. Tooth Extraction
Extraction is a common procedure for wisdom teeth associated with recurrent pericoronitis. The procedure involves:
Administering local anesthesia or sedation for comfort.
Carefully removing the tooth and cleaning the socket to prevent infection.
Providing post-extraction care instructions to promote healing.
3. Post-Extraction Care
Following tooth removal, patients are advised to:
Avoid strenuous activities for the first 24 hours.
Eat soft foods and avoid hot or spicy items that may irritate the extraction site.
Maintain oral hygiene but avoid brushing directly over the surgical site for a few days.
4. Preventive Measures
In cases where extraction isn’t performed, regular monitoring and preventive care, such as periodic cleaning or operculectomy, can help manage the condition effectively.
FAQs about Pericoronitis
1. Can pericoronitis heal on its own?
Mild cases of pericoronitis can sometimes resolve on their own with proper oral hygiene and care. Steps you can take include:
Rinsing with Warm Salt Water: This helps reduce bacteria and inflammation.
Maintaining Oral Hygiene: Brush and floss gently around the affected area to prevent further irritation.
Avoiding Irritants: Stay away from hard or spicy foods that might worsen the condition.
However, if the condition persists or worsens, professional treatment is necessary. Severe cases often require dental intervention, such as cleaning, drainage, or even tooth extraction.
2. How do you know if it is pericoronitis?
Pericoronitis occurs when the gum tissue surrounding a partially erupted tooth, often a wisdom tooth, becomes inflamed. Common symptoms include:
Pain or Swelling: Around the affected tooth, typically in the back of the mouth.
Red or Inflamed Gums: The gums may appear swollen and tender.
Difficulty Opening Mouth (Trismus): Pain or discomfort when trying to open the mouth fully.
Bad Breath or Taste: Due to trapped food particles and bacteria.
Pus or Infection Signs: In severe cases, you may notice discharge.
A dentist can confirm pericoronitis through a physical examination and possibly X-rays.
3. How urgent is pericoronitis?
The urgency of treatment depends on the severity:
Mild Cases: Can often be managed with home care and routine dental visits.
Moderate Cases: Require prompt attention to prevent complications, including antibiotics or cleaning to control infection.
Severe Cases: An emergency, particularly if the infection spreads, causing swelling, fever, or difficulty breathing. Immediate professional care is essential to avoid potentially serious health risks.