Chronic periodontitis is a common and serious gum disease that can lead to significant oral health issues, including tooth loss, if left untreated. It’s important to recognize the signs of this condition early, as prompt treatment can prevent severe damage to the gums, teeth, and supporting bone structure. While there are various symptoms of chronic periodontitis, two of the most noticeable signs are persistent gum inflammation and gum recession. Understanding these early warning signs can help patients seek timely dental care and manage the disease before it becomes more severe.
In this article, we will explore the nature of chronic periodontitis, its two primary signs—gum inflammation and gum recession—and how recognizing these symptoms can lead to better oral health outcomes. Additionally, we’ll cover the causes, risk factors, and treatment options for chronic periodontitis, as well as why maintaining healthy gums is crucial for overall well-being.
Understanding Chronic Periodontitis
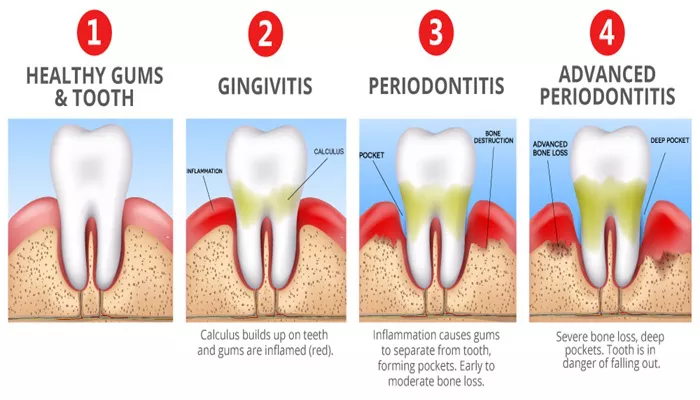
Periodontitis refers to a group of gum diseases that affect the tissues surrounding and supporting the teeth. It occurs when the gums become infected and inflamed due to plaque buildup, which contains harmful bacteria. If left untreated, the infection can cause the gums to recede, and the bone that holds the teeth in place may deteriorate, leading to tooth mobility or loss.
Chronic periodontitis, as the name suggests, is a long-term form of periodontitis that progresses slowly over time. It is the most common form of periodontitis and usually affects adults. However, it can also affect individuals of any age, especially those with poor oral hygiene habits.
The primary cause of chronic periodontitis is the accumulation of plaque and tartar (hardened plaque) along the gumline, which harbors bacteria. The bacteria in this plaque can irritate the gums, leading to inflammation, bleeding, and infection. Without proper treatment, the inflammation can spread, causing damage to the tissues and bones that support the teeth.
Gum Inflammation: A Key Sign of Chronic Periodontitis
One of the most common signs of chronic periodontitis is persistent gum inflammation. This occurs when the gum tissue becomes swollen, red, and irritated due to the ongoing infection caused by bacteria. In the early stages of periodontitis, the gums may bleed easily when brushing or flossing, and there may be tenderness or discomfort around the affected areas.
The inflammation occurs as the body’s immune system responds to the bacteria in the plaque. When the body detects these harmful bacteria, it sends white blood cells to fight the infection. The immune response results in the release of chemicals that cause the gums to become swollen and irritated.
Why Gum Inflammation Happens in Chronic Periodontitis
When plaque and tartar build up on the teeth and gums, they create an environment that is perfect for bacterial growth. These bacteria release toxins that trigger the body’s immune response. As the body tries to fight off the infection, the gums become inflamed. This inflammation can affect the tissues that support the teeth, causing the gums to separate from the teeth and form pockets that can harbor more bacteria.
As the disease progresses, the inflammation becomes more persistent. Without treatment, the infection can spread deeper into the tissues, potentially causing severe damage to the gums and the bone structure that holds the teeth in place.
Symptoms of Gum Inflammation in Chronic Periodontitis:
- Red, swollen, or tender gums
- Gums that bleed easily when brushing or flossing
- Persistent bad breath (halitosis)
- Gum sensitivity, especially when eating or drinking hot or cold foods
Gum inflammation is one of the first signs that chronic periodontitis may be present. If you notice any of these symptoms, it is important to consult a dentist for an evaluation. Early intervention can prevent the disease from progressing to more severe stages.
Gum Recession: A Key Sign of Chronic Periodontitis
Another common sign of chronic periodontitis is gum recession. Gum recession occurs when the gum tissue around the teeth pulls back or wears away, exposing more of the tooth’s surface or the tooth root. As the gums recede, pockets form between the teeth and gums, which can trap food particles and bacteria. These pockets can deepen over time, causing further damage to the gums and the bone structure.
Gum recession is particularly concerning because it can lead to tooth sensitivity. When the roots of the teeth are exposed, they can become more sensitive to temperature changes, such as hot or cold foods and beverages. Additionally, as the gum tissue recedes, the teeth may appear longer, which can affect the overall appearance of the smile.
Why Gum Recession Happens in Chronic Periodontitis
Gum recession occurs as a result of ongoing gum inflammation. When the infection spreads beneath the gum line, it weakens the supporting structures of the tooth, causing the gums to pull away from the teeth. Over time, this can lead to the formation of deep pockets between the gums and teeth, where bacteria can thrive. The bacteria continue to attack the gum tissue and bone, leading to further recession and damage.
Gum recession can also be exacerbated by poor oral hygiene habits, aggressive brushing, or genetic factors. Some individuals may be more susceptible to gum recession due to their genetic makeup, making it more difficult to maintain healthy gum tissue.
Symptoms of Gum Recession in Chronic Periodontitis:
- Gums that appear to pull back or shrink away from the teeth
- Teeth that appear longer than usual
- Increased tooth sensitivity, especially to hot or cold foods
- Visible gaps between the teeth and gums
- Pain or discomfort around the affected teeth
Like gum inflammation, gum recession is a sign of advanced chronic periodontitis. It is essential to address gum recession promptly to prevent further damage to the teeth and gums. Treatment options for gum recession may include deep cleaning (scaling and root planing), gum grafting, or other periodontal procedures to restore gum health.
Causes and Risk Factors for Chronic Periodontitis
Chronic periodontitis is primarily caused by poor oral hygiene that leads to plaque buildup on the teeth and gums. However, several factors can increase the risk of developing this condition:
Poor Oral Hygiene: Inadequate brushing and flossing allow plaque to build up, leading to gum disease.
Tobacco Use: Smoking or chewing tobacco weakens the immune system, making it harder for the body to fight infections.
Genetics: Some individuals are genetically predisposed to developing periodontal disease.
Age: Periodontal disease is more common in adults, particularly those over the age of 30.
Diabetes: Individuals with diabetes are at higher risk for developing periodontitis.
Medications: Certain medications, such as those that cause dry mouth, can increase the risk of gum disease.
Hormonal Changes: Pregnancy, menopause, and other hormonal changes can make the gums more susceptible to inflammation.
Maintaining good oral hygiene, avoiding tobacco use, and managing underlying health conditions are essential for preventing chronic periodontitis.
Treatment for Chronic Periodontitis
Treatment for chronic periodontitis depends on the severity of the disease. Early-stage periodontitis can often be managed with non-surgical treatments, such as:
Scaling and Root Planing: This deep cleaning procedure removes plaque and tartar from beneath the gumline and smooths the tooth surfaces to help the gums reattach.
Antibiotics: Oral or topical antibiotics may be prescribed to help control the bacterial infection.
In more advanced cases, surgical treatments may be necessary, including:
Flap Surgery: This procedure involves lifting the gum tissue to remove tartar and bacteria from deep pockets.
Bone Grafting: If bone loss has occurred, bone grafting can help regenerate lost bone tissue.
Soft Tissue Grafts: Gum grafting can be used to restore gum tissue that has receded.
Regular dental checkups and cleanings are essential for managing and preventing the progression of chronic periodontitis.
Conclusion
Chronic periodontitis is a serious gum disease that can lead to tooth loss and other oral health complications if left untreated. Two primary signs of this condition are persistent gum inflammation and gum recession. These symptoms should not be ignored, as early detection and treatment can prevent further damage and improve long-term oral health.
Maintaining good oral hygiene, seeking professional dental care, and addressing any underlying health issues are key to preventing chronic periodontitis. If you notice any signs of gum disease, including swelling, bleeding, or gum recession, schedule a visit to your dentist as soon as possible. Timely treatment can help protect your teeth, gums, and overall health for years to come.