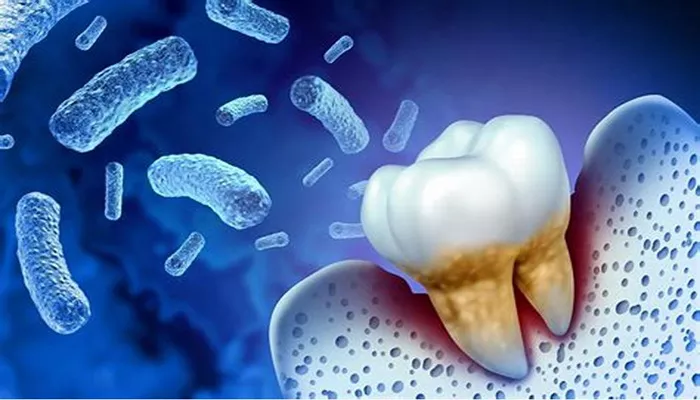
Periodontal disease, also known as gum disease, is a common condition that affects the tissues surrounding the teeth. It is caused by bacterial infection, and if left untreated, it can lead to tooth loss and other serious health problems. One of the most crucial factors in understanding and managing periodontal disease is knowing which bacteria are responsible for causing the infection. In this article, we will explore the primary bacteria associated with periodontal disease, how they contribute to the condition, and what can be done to prevent and treat it.
Introduction to Periodontal Disease
Periodontal disease is an infection of the gums and supporting structures of the teeth. It typically begins with gingivitis, which is the inflammation of the gums caused by plaque buildup. If not treated, gingivitis can progress to periodontitis, a more severe form of the disease that affects the bone and tissue supporting the teeth. Periodontal disease is one of the leading causes of tooth loss among adults, and it has been linked to other serious health issues, such as heart disease, diabetes, and stroke.
The root cause of periodontal disease is the accumulation of plaque—a sticky film of bacteria that forms on the teeth. When plaque is not removed through proper brushing and flossing, it hardens into tartar, which can only be removed by a dental professional. As plaque and tartar build up, the bacteria begin to attack the gums, leading to inflammation, infection, and eventually damage to the bone and other tissues.
But what exactly are these bacteria, and how do they contribute to the development of periodontal disease? Let’s take a closer look at the main bacteria involved in this condition.
The Main Bacteria Causing Periodontal Disease
The development of periodontal disease is primarily driven by the presence of certain types of bacteria in the mouth. These bacteria are able to invade the gums and cause inflammation, infection, and destruction of the supporting tissues. The following are the key bacteria responsible for periodontal disease:
1. Porphyromonas gingivalis (P. gingivalis)
Porphyromonas gingivalis is considered one of the most harmful and influential bacteria in the development of periodontal disease. It is a gram-negative, anaerobic bacterium, meaning it thrives in environments with little to no oxygen. P. gingivalis is found in high numbers in the dental plaque of individuals with periodontitis. It is highly virulent, meaning it is capable of causing significant damage to the gums and supporting structures of the teeth.
P. gingivalis produces various enzymes that break down the tissues in the gums, leading to inflammation and tissue destruction. This bacterium also has the ability to evade the immune system, allowing it to persist and continue causing harm over time. Additionally, P.
gingivalis has been linked to other systemic diseases, including heart disease and diabetes, making it a serious health concern.
2. Tannerella forsythia (T. forsythia)
Tannerella forsythia is another gram-negative bacterium that plays a significant role in the development of periodontal disease. Like P. gingivalis, T. forsythia thrives in anaerobic conditions and is often found in high concentrations in individuals with periodontitis. This bacterium is associated with more severe forms of periodontal disease and is commonly found in deeper pockets of infected gums.
T. forsythia produces enzymes that help break down collagen, a key structural protein in the gums. This leads to the breakdown of gum tissue and the formation of periodontal pockets, which are spaces between the gums and teeth that fill with bacteria and pus. T. forsythia also contributes to the formation of biofilms, which are communities of bacteria that are difficult for the immune system to clear and can contribute to chronic infections.
3. Treponema denticola (T. denticola)
Treponema denticola is a spirochete bacterium that is closely associated with periodontal disease, especially in cases of aggressive periodontitis. It is a motile, anaerobic organism that is capable of penetrating and colonizing the gums, where it can cause inflammation and tissue destruction. T. denticola is often found in combination with P. gingivalis and T. forsythia, forming what is known as the “red complex” of bacteria, which is a group of microorganisms strongly linked to the development of periodontal disease.
T. denticola is particularly harmful because of its ability to produce enzymes that degrade the tissue and interfere with the immune system’s ability to fight the infection. This bacterium is often found in the deeper pockets of infected gums, where it can cause more significant damage to the bone and soft tissues.
4. Fusobacterium nucleatum (F. nucleatum)
Fusobacterium nucleatum is another important bacterium in the development of periodontal disease. It is a gram-negative anaerobic bacterium that acts as a “bridge” between early and late colonizers of the dental plaque. F. nucleatum is capable of promoting the growth of other harmful bacteria, such as P. gingivalis, by creating an environment conducive to their growth.
While F. nucleatum itself is not as destructive as some of the other bacteria mentioned, it plays a crucial role in the progression of periodontal disease by facilitating the colonization of other more pathogenic bacteria. F. nucleatum has also been associated with systemic conditions like cardiovascular disease and pregnancy complications, further emphasizing its potential health risks.
5. Aggregatibacter actinomycetemcomitans (A. actinomycetemcomitans)
Aggregatibacter actinomycetemcomitans is a bacterium that is often found in the mouths of individuals with aggressive periodontitis, a more severe form of periodontal disease that typically affects younger individuals. It is a gram-negative, facultative anaerobe, meaning it can survive in both oxygen-rich and oxygen-poor environments.
A. actinomycetemcomitans is particularly harmful because it produces toxins that damage the gums and bone. It is also capable of evading the immune system, which allows the infection to persist and worsen over time. The presence of A. actinomycetemcomitans is often a marker for more aggressive forms of periodontal disease, which can result in significant tooth loss if not treated properly.
How Do These Bacteria Cause Periodontal Disease?
The bacteria responsible for periodontal disease are able to cause damage in several ways:
Infection and Inflammation: When the bacteria build up on the teeth, they create an infection that triggers an inflammatory response in the gums. This inflammation is the body’s natural defense mechanism, but it can also lead to the destruction of gum tissue and bone.
Toxin Production: Many of the bacteria involved in periodontal disease produce toxins that damage the gums and other tissues. These toxins can also impair the body’s immune response, making it more difficult for the body to fight the infection.
Collagen Breakdown: Some of the bacteria, such as T. forsythia and T. denticola, produce enzymes that break down collagen, a key component of gum tissue. This leads to the formation of deep pockets between the gums and teeth, where bacteria can thrive and cause further damage.
Immune System Evasion: The bacteria responsible for periodontal disease are often able to evade the immune system, allowing them to persist and continue causing damage over time. This is why periodontal disease can become chronic if not properly managed.
Preventing and Treating Periodontal Disease
The best way to prevent periodontal disease is by maintaining good oral hygiene. This includes brushing your teeth twice a day, flossing daily, and visiting the dentist regularly for cleanings and check-ups. If you are already showing signs of gum disease, such as bleeding gums or bad breath, it is important to seek treatment as soon as possible to prevent the condition from progressing.
Treatment for periodontal disease may involve professional cleanings to remove plaque and tartar, scaling and root planing to smooth the roots of the teeth and promote healing, or even surgical procedures in more advanced cases.
In addition to professional treatments, patients may be advised to use antibacterial mouthwashes or medications to help control the bacterial infection and promote healing.
Conclusion
Periodontal disease is a serious condition that can lead to tooth loss and other health complications if left untreated. The main bacteria responsible for causing periodontal disease are Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola, Fusobacterium nucleatum, and Aggregatibacter actinomycetemcomitans. These bacteria contribute to the disease by producing toxins, breaking down gum tissue, and evading the immune system.
Understanding these bacteria and their role in periodontal disease is essential for preventing and treating this condition. By practicing good oral hygiene and seeking prompt dental care, individuals can reduce their risk of developing periodontal disease and maintain healthy gums and teeth.