Periodontal disease, also known as gum disease, is a serious oral health condition that affects the tissues surrounding and supporting the teeth. If left untreated, it can lead to tooth loss and may even increase the risk of other systemic diseases, such as heart disease and diabetes. Periodontal disease usually begins with gingivitis, a mild form of gum disease that causes irritation, redness, and swelling of the gums. When gingivitis progresses, it can lead to periodontitis, a more severe form of the disease that affects the deeper tissues of the teeth and gums.
The good news is that periodontal disease is preventable and treatable. Early diagnosis and prompt treatment can help restore oral health and prevent further complications. In this article, we will explore the 10 best treatments for periodontal disease, ranging from basic at-home care to more advanced professional procedures.
1. Professional Cleaning (Scaling and Root Planing)
One of the most effective treatments for periodontal disease is professional cleaning, also known as scaling and root planing. This non-surgical procedure is typically performed by a dental hygienist or periodontist. It involves removing plaque and tartar (hardened plaque) from the surface of the teeth and below the gumline. The process also includes smoothing the root surfaces to help the gums reattach to the teeth, preventing bacteria from accumulating in the area.
Scaling and root planing are usually the first line of treatment for patients with mild to moderate periodontitis. This treatment is highly effective in reducing the depth of periodontal pockets and promoting gum healing. It is often followed by a maintenance plan of regular cleanings to keep the disease from progressing.
2. Antimicrobial Treatments
In addition to professional cleaning, antimicrobial treatments can help control the bacteria responsible for periodontal disease. These treatments can be applied directly to the gums and teeth in the form of mouth rinses, gels, or localized antibiotics. Some of the most common antimicrobial treatments include:
Chlorhexidine: An antiseptic mouth rinse that helps kill bacteria and reduce inflammation in the gums.
Arestin: An antibiotic gel that is placed directly into the periodontal pockets to fight bacteria and reduce gum infection.
Peridex: A mouth rinse containing chlorhexidine that is often prescribed after scaling and root planing to reduce bacteria and inflammation.
These antimicrobial treatments can be especially useful for individuals who have pockets of infection that are difficult to treat with cleaning alone. They help reduce the bacterial load and promote faster healing.
3. Laser Therapy
Laser therapy is a relatively new treatment option for periodontal disease, and it has shown promising results in many cases. This procedure uses a focused laser beam to remove infected tissue and bacteria from the periodontal pockets while preserving healthy tissue. The laser also stimulates the regeneration of gum tissue and promotes healing.
Laser therapy offers several benefits over traditional treatments, including:
Reduced pain and discomfort during and after the procedure
Faster recovery time
Less bleeding compared to traditional surgical methods
Precision in targeting infected tissue without harming healthy areas
Laser therapy is typically used for moderate to advanced periodontal disease and may be combined with scaling and root planing for more effective results.
4. Periodontal Surgery
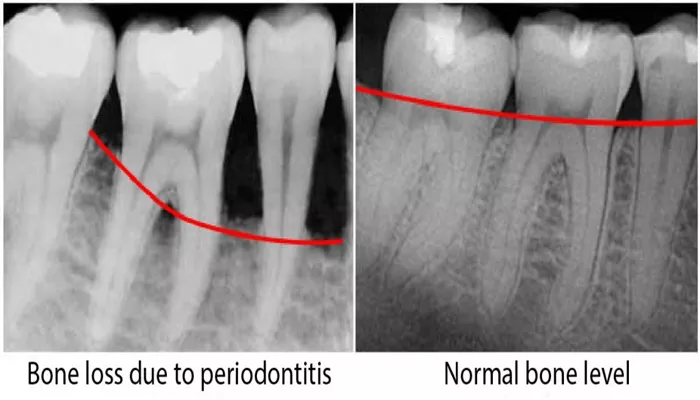
For severe cases of periodontal disease that do not respond to nonsurgical treatments, periodontal surgery may be necessary. The goal of surgery is to reduce the size of periodontal pockets, remove damaged tissue, and regenerate bone that may have been lost due to infection.
There are several types of periodontal surgery, including:
Flap Surgery: In this procedure, the gums are lifted back to allow access to the roots and bone for cleaning. Once the infection is cleared, the gums are repositioned to fit snugly around the teeth.
Bone Grafting: If bone loss has occurred due to periodontal disease, bone grafting may be recommended. This involves placing bone material (either from the patient or a donor) into the affected area to help regenerate lost bone tissue.
Tissue Grafting: In cases where gum tissue has been lost, a gum graft may be performed to restore the tissue and reduce gum recession.
Periodontal surgery is typically recommended for patients with advanced periodontitis who have not responded to nonsurgical treatments.
5. Dental Implants
For patients with severe gum disease that has resulted in tooth loss, dental implants may be an ideal treatment option.
Dental implants are titanium posts that are surgically placed into the jawbone to replace missing teeth. Once the implant has fused with the bone, a crown is placed on top to restore the appearance and function of the missing tooth.
Dental implants not only improve the aesthetic appearance of the smile but also help restore proper chewing function.
Moreover, implants can prevent further bone loss in the jaw, which can occur after tooth loss. However, good oral hygiene is crucial to the long-term success of implants, as they can still be affected by periodontal disease if not properly cared for.
6. Oral Hygiene Education
One of the most important components of treating and preventing periodontal disease is good oral hygiene. Patients with periodontal disease need to be educated on the importance of brushing, flossing, and regular dental visits. Proper oral care at home can help reduce plaque buildup, control bacteria, and prevent the progression of gum disease.
Some key oral hygiene tips include:
Brushing: Use a soft-bristled toothbrush and fluoride toothpaste to brush your teeth at least twice a day. Be sure to brush all surfaces, including the gumline, where plaque and bacteria tend to accumulate.
Flossing: Floss at least once a day to remove plaque and food particles from between the teeth and below the gumline, areas that a toothbrush cannot reach.
Mouthwash: Use an antimicrobial or fluoride mouthwash to reduce plaque buildup and strengthen teeth.
Education on proper oral hygiene is an essential part of any periodontal treatment plan to ensure long-term success.
7. Smoking Cessation Programs
Smoking is a major risk factor for periodontal disease. It weakens the immune system, making it harder for the body to fight off infections, and it reduces blood flow to the gums, slowing down the healing process. Smoking also promotes the growth of harmful bacteria in the mouth, further aggravating gum disease.
For patients who smoke, quitting is one of the most important steps they can take to improve their oral health and prevent further progression of periodontal disease. Smoking cessation programs, counseling, and nicotine replacement therapies can be helpful in quitting smoking and improving overall gum health.
8. Maintenance Cleanings
After the initial treatment for periodontal disease, regular maintenance cleanings are essential to prevent the disease from returning. These cleanings are typically performed every 3 to 4 months and involve thorough scaling and polishing to remove any plaque or tartar buildup.
Maintenance cleanings also allow the dentist to monitor the patient’s progress and address any emerging issues before they become serious.
For individuals with a history of periodontal disease, these frequent cleanings are crucial in maintaining good oral health and preventing the need for more aggressive treatments.
9. Antibiotic Therapy
In certain cases, oral antibiotics may be prescribed to help manage periodontal disease, especially if the infection is widespread or if the patient is not responding to other treatments. Antibiotics can be taken orally or applied topically to the gums to target specific bacteria.
Common antibiotics used for periodontal disease include:
Amoxicillin: A broad-spectrum antibiotic often used to treat bacterial infections in the mouth.
Doxycycline: A type of tetracycline antibiotic that helps reduce inflammation and bacterial growth in the gums.
Antibiotics are usually used in conjunction with other treatments, such as scaling and root planing, to help control the infection and promote healing.
10. Systemic Health Management
Managing systemic health conditions, such as diabetes and heart disease, is crucial in the treatment of periodontal disease.
These conditions can worsen periodontal disease by affecting the body’s ability to fight infections and heal. By controlling blood sugar levels in diabetic patients or managing cardiovascular risk factors, patients can reduce the severity of gum disease and improve their overall oral health.
For patients with underlying health conditions, a collaborative approach between their dentist and primary care physician is essential to ensure optimal treatment outcomes.
Conclusion
Periodontal disease is a common yet serious condition that can affect anyone. Fortunately, there are numerous effective treatments available to manage and treat gum disease, ranging from professional cleaning and antimicrobial therapies to surgical procedures and lifestyle changes. Early intervention is key to preventing further damage and ensuring long-term oral health.