Pulp infection, often referred to as pulpitis, is a serious dental condition that arises from inflammation of the dental pulp.
The dental pulp is the innermost part of the tooth, containing vital components such as blood vessels, nerves, and connective tissue. This soft tissue plays a crucial role in maintaining the health of the tooth by providing nourishment and sensory functions. When the dental pulp becomes inflamed or infected, it can lead to significant pain and discomfort, affecting an individual’s overall oral health. This article delves into the causes, symptoms, diagnosis, treatment options, and preventive measures associated with pulp infection.
What Is Pulp Infection?
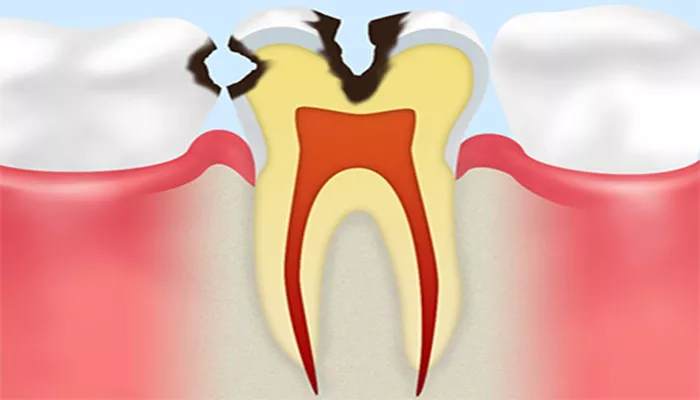
Pulp infection occurs when bacteria invade the dental pulp, leading to inflammation and potential necrosis (death) of the pulp tissue. The most common cause of this condition is untreated dental caries (tooth decay), which allows bacteria to penetrate through the protective enamel and dentin layers of the tooth. Other contributing factors include trauma to the tooth, multiple restorations, and parafunctional habits such as teeth grinding (bruxism).
The inflammation associated with pulp infection can be classified into two main types: reversible pulpitis and irreversible pulpitis. Reversible pulpitis is characterized by mild inflammation that can heal if the irritant is removed, typically through restorative procedures like fillings. In contrast, irreversible pulpitis indicates severe damage to the dental pulp that cannot heal on its own, often necessitating more invasive treatments such as root canal therapy or extraction.
Causes of Pulp Infection
Several factors can lead to pulp infection:
Dental Caries: The primary cause of pulp infection is tooth decay.
Bacteria from plaque buildup produce acids that erode enamel and dentin, eventually reaching the pulp.
Trauma: Physical injuries to the teeth from accidents or sports can crack or fracture teeth, allowing bacteria to enter.
Defective Restorations: Old fillings or crowns that fail can create pathways for bacteria to invade the pulp.
Bruxism: Grinding teeth can wear down enamel and dentin, increasing vulnerability to infection.
Symptoms of Pulp Infection
The symptoms of pulp infection can vary depending on whether it is reversible or irreversible:
Reversible Pulpitis Symptoms:
- Sensitivity to hot or cold stimuli that subsides quickly
- Sharp pain when consuming sweet foods
- Mild discomfort when biting down
- No spontaneous pain
Irreversible Pulpitis Symptoms:
- Severe and persistent toothache that may be spontaneous
- Prolonged sensitivity to temperature changes
- Pain when pressure is applied (e.g., tapping)
- Swelling in surrounding gums
- Possible fever and bad breath
- Tooth discoloration
In some cases, individuals may not experience any symptoms until the infection progresses significantly.
Diagnosis of Pulp Infection
Diagnosing pulp infection typically involves a comprehensive evaluation by a dentist. The diagnostic process may include:
Clinical Examination: The dentist will assess symptoms and perform a physical examination of the affected tooth.
Pulp Vitality Tests: These tests involve applying thermal stimuli (cold or heat) or electric pulses to determine if the dental pulp is alive.
Radiographic Imaging: X-rays are crucial for visualizing the extent of decay and any bone loss surrounding the tooth due to infection.
Treatment Options for Pulp Infection
Treatment for pulp infection depends on its severity:
Reversible Pulpitis Treatment:
- Removal of decay followed by restoration with a filling
- Improved oral hygiene practices
- Regular dental check-ups to monitor tooth health
Irreversible Pulpitis Treatment:
Root Canal Therapy: This procedure involves removing infected pulp tissue, cleaning and disinfecting the root canals, and sealing them with a biocompatible material. A crown may be placed afterward for protection.
Tooth Extraction: If the tooth is severely damaged or cannot be saved through root canal therapy, extraction may be necessary.
Complications of Untreated Pulp Infection
If left untreated, pulp infections can lead to serious complications:
Dental Abscess: An accumulation of pus at the root tip can form, leading to intense pain and swelling. This condition may require surgical intervention.
Spread of Infection: In severe cases, bacteria can spread beyond the tooth into surrounding tissues or even systemic circulation, leading to serious health risks such as cellulitis or sepsis.
Preventive Measures for Pulp Infection
Preventing pulp infection largely revolves around maintaining good oral hygiene practices:
Regular Dental Check-Ups: Visiting a dentist every six months for professional cleanings and examinations helps catch issues early before they escalate.
Proper Oral Hygiene: Brushing teeth twice daily with fluoride toothpaste and flossing regularly are essential for reducing plaque buildup.
Dietary Choices: Limiting sugary snacks and beverages helps decrease the risk of developing cavities that could lead to pulp infections.
Protective Gear: Using mouthguards during sports can prevent trauma-related injuries to teeth.
Conclusion
Pulp infection is a significant dental issue that requires prompt attention to prevent complications. Understanding its causes, symptoms, diagnosis methods, treatment options, and preventive strategies is crucial for maintaining oral health.
Individuals should prioritize regular dental visits and practice good oral hygiene to reduce their risk of developing this painful condition. If you experience any symptoms indicative of pulp infection, seek professional dental care immediately for appropriate diagnosis and treatment.