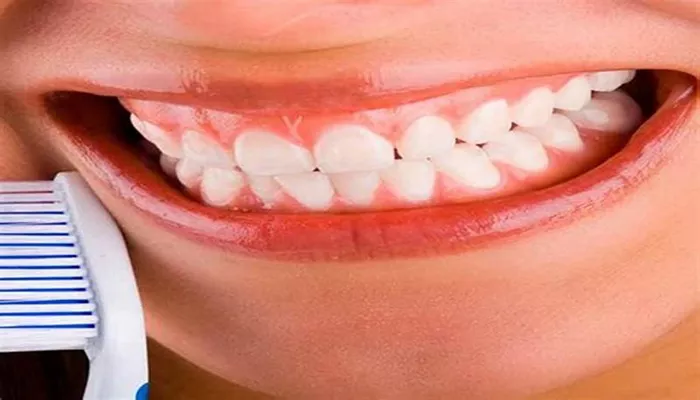
Gingivitis is a common and mild form of gum disease (periodontal disease) that causes irritation, redness, and swelling (inflammation) of your gingiva, the part of your gum around the base of your teeth. It is the earliest stage of gum disease and is primarily caused by poor oral hygiene that encourages plaque to form on teeth, causing inflammation of the surrounding gum tissue. In this article, we’ll explain what gingivitis looks like, what causes it, and how you can prevent and treat it effectively.
What Are The Symptoms of Gingivitis?
Gingivitis can be difficult to notice in its early stages, but there are several symptoms and signs that can help identify it.
These symptoms often become more apparent if the condition progresses without treatment. Here are some of the key signs and symptoms that indicate you might have gingivitis:
1. Red, Swollen Gums
One of the first signs of gingivitis is that your gums may become red and swollen. Healthy gums are usually pale pink, but when they are inflamed, they may appear bright red or dark red. Inflammation causes the blood vessels in the gums to dilate, making them look more noticeable.
2. Bleeding Gums
Bleeding is another hallmark of gingivitis. Gums that are inflamed and irritated often bleed easily when brushing or flossing. You may notice small amounts of blood in the sink after brushing or when you spit. If your gums are bleeding frequently, it is a sign that you may be developing gingivitis.
3. Tender Gums
Your gums may feel tender or sore to the touch. This tenderness can be triggered by brushing your teeth, chewing, or even gentle pressure from your toothbrush. In the case of gingivitis, the gums are inflamed and may become more sensitive than usual.
4. Bad Breath (Halitosis)
Persistent bad breath, also known as halitosis, is another common symptom of gingivitis. The bacteria that cause gingivitis can produce foul-smelling compounds that result in a bad odor in your mouth. If you notice a persistent bad taste or odor, this could be a sign that gingivitis is present.
5. Receding Gums
In more advanced cases of gingivitis, you may notice that your gums appear to be shrinking or pulling away from your teeth.
This recession exposes more of your teeth or the tooth’s roots. Receding gums can cause discomfort and make your teeth more sensitive to hot and cold temperatures.
6. Soft or Puffy Gums
Gums that are soft, swollen, and puffy can be a sign of gingivitis. Healthy gums should fit snugly around the teeth, but inflamed gums often appear more swollen and larger in size, making the gum line look uneven.
7. Changes in the Texture of Gums
As gingivitis develops, your gums may take on an unusual texture. Instead of appearing smooth, they may appear rough or bumpy due to the inflammation. This texture change is often caused by the excess plaque or tartar buildup that leads to gum irritation.
What Causes Gingivitis?
Gingivitis is primarily caused by the accumulation of plaque—a sticky, colorless film of bacteria that forms on your teeth and gums. Plaque is constantly forming in your mouth, but when it is not removed by regular brushing and flossing, it can harden into tartar (calculus) which can irritate the gums and lead to gingivitis.
Here are some specific reasons for the development of gingivitis:
1. Poor Oral Hygiene Habits
The most common cause of gingivitis is poor oral hygiene that encourages plaque to form on teeth and gums. If you don’t brush and floss regularly, plaque can harden into tartar, which irritates the gums. Over time, tartar buildup leads to chronic inflammation and gingivitis.
2. Smoking or Chewing Tobacco
Tobacco use is another significant risk factor for gingivitis. Smoking and chewing tobacco can make it harder for your gums to heal and increase the risk of developing gingivitis. Smoking also reduces blood flow to the gums, which can impair the body’s ability to fight infections and heal gum tissue.
3. Poor Nutrition
A poor diet lacking in essential nutrients, particularly vitamin C, can also increase the risk of gingivitis. Vitamin C is crucial for the health of your gums, and a deficiency can lead to weakened gum tissue that is more susceptible to infection and inflammation.
4. Certain Medications
Some medications can have side effects that make gingivitis more likely. Medications that reduce saliva flow (such as antihistamines, decongestants, and medications for high blood pressure) can lead to dry mouth. Saliva helps wash away food particles and bacteria, and when saliva production is reduced, plaque can accumulate more easily on the gums.
5. Conditions that Affect Immune Function
Conditions such as diabetes, HIV/AIDS, and cancer treatment can affect the immune system, making it harder for your body to fight infections. A weakened immune system increases the risk of developing gum disease, including gingivitis.
6. Age
As you age, your risk of developing gingivitis increases.
Older adults may experience more difficulty with oral hygiene due to physical limitations, such as arthritis in the hands or other health issues. Additionally, age-related changes in saliva production or tooth alignment can make it harder to clean the teeth and gums properly.
7. Hormonal Changes
Changes in hormone levels, such as those that occur during pregnancy, menstruation, or menopause, can make the gums more sensitive and prone to irritation. During pregnancy, for example, hormonal fluctuations can increase blood flow to the gums, causing them to become swollen, red, and more susceptible to gingivitis.
8. Dental Fillings or Crowns That Don’t Fit Properly
Ill-fitting dental restorations, such as fillings or crowns, can cause food and plaque to become trapped in areas that are difficult to clean. If these restorations do not fit properly, they can cause irritation to the surrounding gum tissue and contribute to the development of gingivitis.
9. Medical Conditions
Certain medical conditions, including viral infections and certain genetic conditions, can increase the risk of gingivitis. For example, people with a history of heart disease or stroke may be at greater risk for gum problems, including gingivitis, as inflammation in the mouth can contribute to systemic health issues.
How to Prevent Gingivitis?
Prevention is the key to avoiding gingivitis and ensuring that your gums stay healthy. Here are some essential steps to help you prevent gingivitis:
1. Brush Your Teeth Twice a Day
Brushing your teeth at least twice a day is one of the best ways to prevent gingivitis. Make sure to use a fluoride toothpaste and a soft-bristled toothbrush to clean your teeth. Pay special attention to the gum line to remove plaque buildup that can lead to gingivitis.
2. Floss Daily
Flossing helps remove plaque and food particles between your teeth and along the gumline, areas that your toothbrush may miss. Flossing at least once a day can significantly reduce the risk of gingivitis.
3. Visit Your Dentist Regularly
Regular dental checkups and cleanings are essential for preventing gingivitis. Your dentist or dental hygienist can remove plaque and tartar that have built up on your teeth and gums, which can help reduce your risk of developing gum disease.
4. Use Mouthwash
Using an antimicrobial mouthwash can help reduce the bacteria that cause gingivitis. Mouthwash can reach areas that your toothbrush and floss might miss, providing extra protection for your gums.
5. Quit Smoking
If you smoke or use tobacco, quitting can significantly reduce your risk of gingivitis and other oral health problems. Tobacco use weakens your immune system and can make it harder for your gums to heal, increasing the risk of gum disease.
6. Eat a Balanced Diet
Eating a diet rich in vitamins and minerals, particularly vitamin C, can help support healthy gums. Foods such as fruits, vegetables, and lean proteins are essential for overall oral health.
Conclusion
Gingivitis is a common and treatable condition, but it can lead to more serious gum disease if left untreated. Recognizing the signs of gingivitis—such as red, swollen gums, bleeding, bad breath, and tenderness—can help you address the problem before it progresses. Maintaining good oral hygiene, quitting smoking, and visiting your dentist regularly are the most effective ways to prevent and treat gingivitis.