types of gum disease
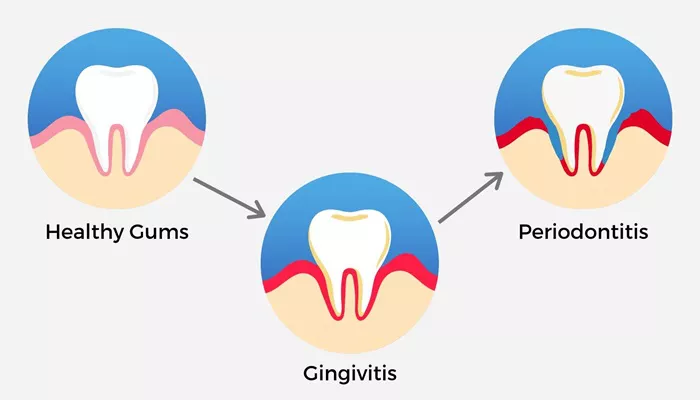
1. Gingivitis: The Early Stage of Gum Disease
Gingivitis is the mildest form of gum disease and the first stage in the development of periodontal disease. It is characterized by inflammation and irritation of the gums, which may become red, swollen, and bleed easily when brushing or flossing.
Gingivitis occurs when plaque accumulates along the gumline. Plaque contains bacteria that irritate the gums, leading to their swelling. If caught early, gingivitis is reversible with professional cleaning by a dentist and improved at-home oral care.
Symptoms of Gingivitis:
Red, swollen, or puffy gums
Gums that bleed easily when brushing or flossing
Bad breath (halitosis)
Mild gum pain or discomfort
A receding gumline (in some cases)
If gingivitis is not addressed, it can progress to more serious forms of gum disease.
2. Periodontitis: A More Advanced Form of Gum Disease
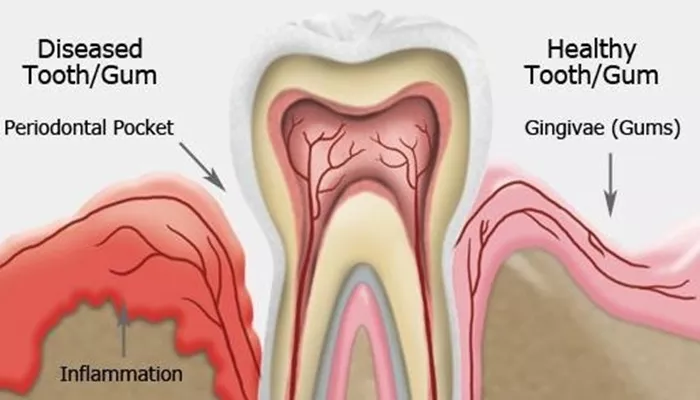
If gingivitis is left untreated, it can lead to periodontitis, which is a more serious and advanced stage of gum disease. In periodontitis, the infection extends deeper into the tissues, causing the gums to pull away from the teeth and form pockets of infection. This can lead to the breakdown of the bone and connective tissue that supports the teeth, ultimately causing tooth mobility or loss.
There are different forms of periodontitis, which include:
Chronic Periodontitis: The most common form of periodontitis, chronic periodontitis usually affects adults, but it can occur at any age. It is characterized by gum recession, pocket formation, and loss of tooth-supporting bone. Chronic periodontitis tends to progress slowly, although it can cause significant damage if left untreated.
Aggressive Periodontitis: This is a rarer, but more severe, form of periodontitis that progresses rapidly, often in otherwise healthy individuals. Aggressive periodontitis typically affects younger people and may cause early tooth loss. It is often characterized by severe gum inflammation, rapid bone loss, and deep periodontal pockets.
Necrotizing Periodontal Disease: This is a severe form of gum disease that causes tissue death in the gums, ligaments, and bone. It is often seen in individuals with compromised immune systems, such as those with HIV/AIDS, malnutrition, or other serious health conditions. Necrotizing periodontal disease requires immediate medical attention.
Symptoms of Periodontitis:
Gums that recede or pull away from the teeth
Persistent bad breath or a bad taste in the mouth
Red, swollen, or bleeding gums
Tender or painful gums
Loose teeth or changes in bite alignment
Formation of pockets between the teeth and gums
Gum abscesses or pus drainage
gum disease symptoms
1. Gum bleeding: Gums that bleed easily during brushing or flossing are a classic sign of gingivitis. If bleeding persists or worsens, it may indicate the progression of gum disease.
2. Red, swollen, or puffy gums: Inflamed gums are a key symptom of gingivitis and periodontitis. Healthy gums should be firm and pale pink.
Bad breath: Chronic bad breath, or halitosis, can be a sign of gum disease. The bacteria in infected gums produce sulfur compounds that cause unpleasant odors.
3. Receding gums: As gum disease progresses, the gums may begin to pull away from the teeth, exposing more of the tooth and its root. This can lead to sensitivity and discomfort.
4. Loose teeth: In advanced stages of periodontitis, the teeth may loosen due to the destruction of the supporting bone and tissues. This can affect the bite and may require professional intervention.
5. Pus or abscesses: The presence of pus or abscesses around the gums is a sign of infection. This can indicate the development of periodontitis or necrotizing periodontal disease.
gum disease causes
1. Poor Oral Hygiene Habits:
Not brushing and flossing regularly allows plaque to harden into tartar. Plaque and tartar harbor harmful bacteria that can infect the gums. Over time, if not removed through regular brushing and professional dental cleanings, these bacteria can lead to gum disease.
2. Smoking and Tobacco Use:
Smoking is a major risk factor for the development of gum disease. Tobacco use weakens the immune system, making it harder for the body to fight off gum infections. Smokers are also more likely to have deeper pockets in their gums and more severe gum disease.
3. Poor Nutrition:
A diet lacking in essential nutrients, particularly vitamin C, can impair the body’s ability to fight off infection. Malnutrition and deficiencies in vitamins and minerals can weaken the gums and increase susceptibility to gum disease.
4. Medical Conditions:
Certain health conditions and diseases can make individuals more vulnerable to gum disease. These include:
Diabetes: People with uncontrolled diabetes are at an increased risk of gum disease because high blood sugar levels can impair the body’s ability to fight infections.
Hormonal changes: Pregnancy, menopause, and puberty can cause changes in the gums, making them more susceptible to gum disease.
Autoimmune diseases: Conditions like rheumatoid arthritis and HIV/AIDS can weaken the immune system and make it harder for the body to fight off infections.
5. Medications:
Some medications, such as those that cause dry mouth or affect the body’s immune system, can increase the risk of gum disease. Dry mouth, in particular, reduces saliva flow, which helps protect the gums and teeth from bacteria.
6. Genetics:
Some individuals may have a genetic predisposition to gum disease, making them more susceptible to developing it, regardless of their oral hygiene habits. A family history of gum disease can be an important risk factor.
7. Age:
As people age, the risk of developing gum disease increases. This is partly due to the natural aging process, which can lead to changes in the mouth, including receding gums and a weakened immune response.
gum disease treatment
1. Professional Cleaning (Scaling and Root Planing):
In the early stages of gum disease, professional cleaning is often sufficient to remove plaque and tartar from the teeth and gums. This procedure, called scaling and root planing, involves cleaning below the gumline to remove bacterial deposits and smooth the tooth roots to help the gums reattach.
2. Medications:
For more advanced cases of gum disease, medications may be prescribed to help control infection and reduce inflammation. These may include:
Antibiotic gels or mouth rinses: Applied directly to the gums to help reduce bacterial infection.
Oral antibiotics: Prescribed to help control bacteria in the mouth and prevent the spread of infection.
3. Surgery:
In severe cases of gum disease, surgery may be necessary to repair the damage to the gums and bone. Surgical options include:
Flap surgery: Involves lifting the gums to remove tartar from deep pockets and then stitching the gums back into place.
Bone grafts: Used to restore bone lost due to periodontitis.
Soft tissue grafts: Used to cover exposed tooth roots and reduce further gum recession.
4. Ongoing Maintenance:
Once gum disease is treated, regular dental visits are essential to monitor the health of the gums and prevent recurrence. Patients with a history of gum disease may require more frequent cleanings and ongoing care to maintain their oral health.
Preventing Gum Disease
Preventing gum disease begins with good oral hygiene practices. These include:
Brushing the teeth twice a day with fluoride toothpaste
Flossing daily to remove plaque from between the teeth
Using an antimicrobial mouthwash to reduce bacteria
Avoiding smoking and tobacco use
Eating a balanced diet rich in vitamins and minerals
Visiting the dentist regularly for checkups and professional cleanings